Chronic Lyme Disease
Lyme disease can be very serious. The infection is often multisystemic – involving joints, heart, and the nervous system. Although early recognition and treatment lead to resolution of illness for many patients, there are many who live with persistent, debilitating symptoms, and persistent infection – which ILADS terms chronic Lyme disease.
If Lyme disease is not diagnosed and treated early, the spirochetes can spread and may go into hiding in different parts of the body. Weeks, months or even years later, patients may develop problems with the brain and nervous system, muscles and joints, heart and circulation, digestion, reproductive system, and skin. Symptoms may disappear even without treatment and different symptoms may appear at different times.
Untreated or undertreated Lyme can cause some people to develop severe symptoms that are hard to resolve. This condition may be referred to as post-treatment Lyme disease (PTLD) or chronic Lyme disease (CLD). We don’t know exactly how many people who are diagnosed and treated remain ill.
The International Lyme and Associated Diseases Society (ILADS) published treatment guidelines which contains a rigorous assessment of the evidence and found treatment failure rates ranging from 16% to 39% for early treatment. Estimates for patients with chronic Lyme disease are much higher, ranging from 26% to 50%. (Johnson 2004)
Although experts do not often attribute deaths to Lyme disease, studies have documented at least 23. In 2014, the CDC issued a warning regarding three sudden cardiac deaths related to Lyme carditis.
Despite some skepticism in the medical community, chronic Lyme disease is a growing epidemic in the U.S. This stems partly from the shortcomings of many of the officially recommended Lyme disease tests, which leave too many patients with untreated infections that then become persistent and debilitating.
Chronic Lyme: What happens when Lyme goes untreated?
The Lyme community typically uses the term “chronic Lyme disease” to describe a range of physical, cognitive, and emotional symptoms that crop up after getting Lyme disease and persist for months to years after infection.
The risk of chronic Lyme increases the longer a Lyme infection goes untreated or undertreated. In other words, patients are more likely to recover fully if their Lyme infection is detected and treated as early as possible after the discovery of a tick bite. This stage is usually marked by symptoms such as fevers, chills, muscle aches, and sometimes rashes.
When left untreated or undertreated, however, Lyme disease can spread throughout the body and affect:
The central nervous system (including psychiatric and cognitive effects)
Muscles and joints
Heart and circulation
The reproductive system
Skin
As Lymedisease.org points out, these symptoms can evolve, disappear, and reappear at different times.
The numbers on chronic Lyme
Because Lyme disease is commonly missed or misdiagnosed, statistics vary on how many Lyme patients go on to experience chronic symptoms. The following research nonetheless paints a basic picture of the problem.
An estimated 5-20% of patients may have chronic symptoms after getting Lyme disease, according to the Columbia University Irving Medical Center.
The treatment failure rate for chronic Lyme disease patients was estimated at 26-50% in 2004, compared to 16-39% for early Lyme patients, according to Lymedisease.org.
Up to 15-40% of late-stage Lyme patients develop neurological disorders, which are responsible for many common symptoms of chronic Lyme disease.
Experts don’t know for sure why some people experience persistent symptoms, even with treatment. However, some believe the Lyme infection may trigger an auto-immune response that manifests in the chronic symptoms detailed below.
Source: https://igenex.com/tick-talk/what-are-the-symptoms-of-chronic-lyme-disease/
Chronic Lyme Disease Patients Profoundly Debilitated
Many patients with chronic Lyme disease are profoundly debilitated. Investigators of the four NIH-sponsored retreatment trials documented that the patients’ quality of life was consistently worse than that of control populations and equivalent to that of patients with congestive heart failure. Pain levels were similar to those of post-surgical patients, and fatigue was on par with that seen in multiple sclerosis.
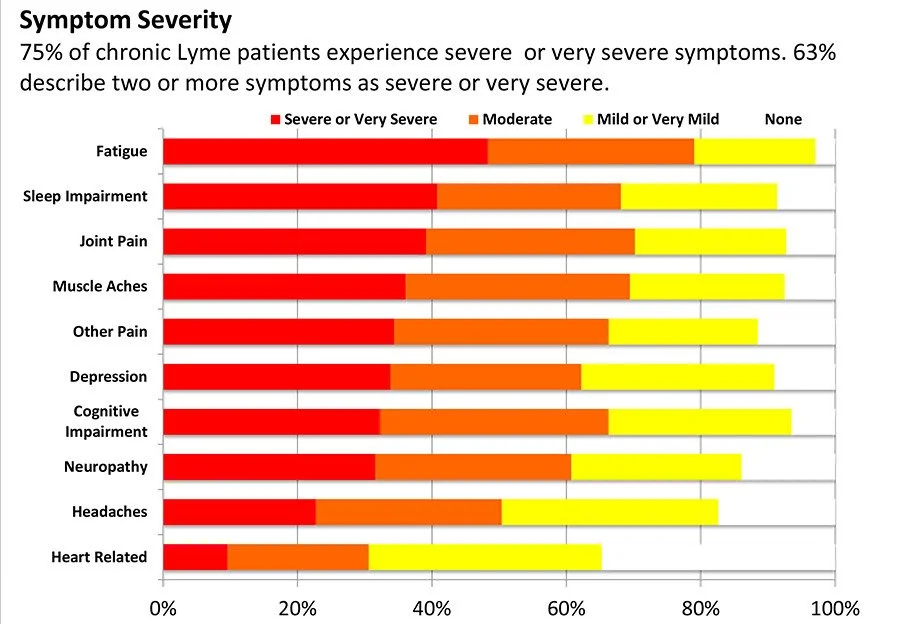
Many of the symptoms associated with Lyme disease are common in other diseases. The CDC surveillance criteria for confirmed cases specifically exclude most of the symptoms that patients report, including fatigue, sleep impairment, joint pain, muscle aches, other pain, depression, cognitive impairment, neuropathy, and headaches. However, these common symptoms can be severe and may seriously affect quality of life.
Chronic Lyme Disease Symptom Severity
In LDo’s chronic Lyme disease survey, over 75% of patients reported at least one symptom as severe or very severe and 63% reported two or more such symptoms. (Johnson 2014) Find out more about LDo peer-reviewed published surveys. The chart below shows the severity of ten common chronic Lyme symptoms.
Controversy over Diagnosis
The controversies in Lyme disease exist in a setting of incomplete scientific evidence around tick-borne diseases, including a lack of validated direct testing methods which can be applied across all stages of the disease to accurately distinguish infected from uninfected patients.
Serologic testing, often held as a gold standard, has significant performance limitations. Lyme disease is a clinical diagnosis dependent on history, and physical examination, and supported by appropriate laboratory testing. The elements of diagnosis are placed in the context of the activities and experiences of the patient, environmental exposures and risk factors, and consideration of other diagnoses that may explain or impact the patient’s symptoms. At the heart of the controversy is the relative weight given to each element that contributes to the diagnosis. ILADS’ position is that no single data point, including serologic testing, automatically outweighs the contributions from all of the data in the patient’s presentation and evaluation.
Issues with diagnosis & diagnostics
There is a distinction between diagnosis and diagnostics. A diagnosis encompasses the considered explanation for a patient’s symptoms based on the elements described above, as well as the process by which the diagnosis itself is reached. Diagnostics refers to laboratory and other test modalities used to aid in reaching a diagnosis. Challenges exist in both areas when considering Lyme disease.
Challenges in diagnosis occur in a setting of varied clinical presentations often appearing in the absence of a history of tick bite. Even the erythema migrans rash (EM), a hallmark of the disease, is not always present or remembered, and in its most common form does not resemble the classically described “bull’s eye” rash.3 The sometimes subtle physical findings and diversity of manifestations of Lyme borreliosis require awareness on the part of the examiner in order to discern this infection. Even in the case of Lyme arthritis with effusion, it has been reported that diagnosis in adults often takes longer than in children.4 In addition, since latency is a feature of this infection, some signs and symptoms do not develop for weeks, months or even years after the time of initial infection.5 6 7 All of these features contribute to diagnostic uncertainties and controversy.
Sources:
https://www.lymedisease.org/lyme-basics/lyme-disease/chronic-lyme-disease/
https://www.ilads.org/research-literature/controversies-challenges/